Ani, mother of a 4-year-old boy, Henry, is in Yerevan to get medical advice over the regular complications observed in her son’s health condition. The frequent increase in the boy’s body temperature seems too risky to keep him in Kapan, the specialists at the pediatric department of the local medical center have told Ani. The head of the department has referred him to examination in one of the Yerevan-based clinics suspecting a kidney dysfunction case.
“We rushed him straight to Arabkir Medical Center. We were supposed to see a nephrologist; but we had to wait in a queue for hours before we could actually see the doctor. The doctors’ suspicions were confirmed; a complication of streptococcal infection has ended up as a kidney dysfunction,” Ani Sargsyan, the boy’s mother, shares with Ampop Media.
The mother and the child are back in Kapan now. Despite Henry has been discharged from the hospital, the health problem may return at any moment; so, Henry remains under doctors’ control at the Arabkir MC.
Nephrologist is not the only specialist required at the Kapan MC. Henry, 4, too, is neither the first, nor the last patient to be rushed to a hospital in Yerevan some 300 kilometers away from his home, because of the lack of specialists in his hometown.
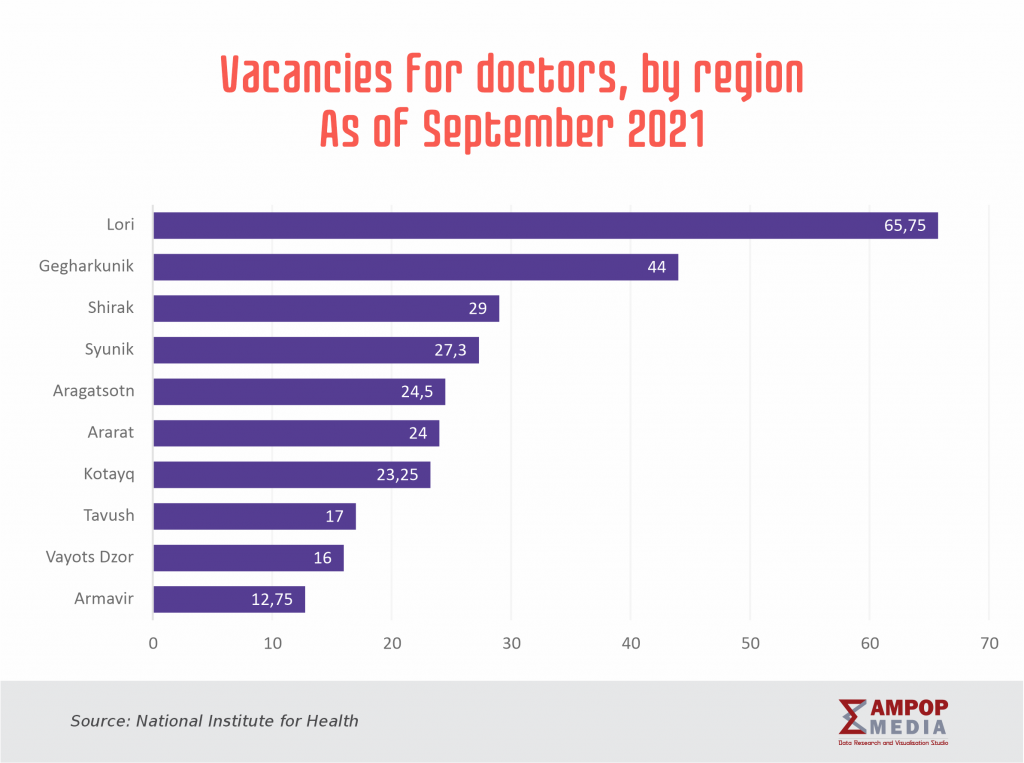
Further yet, the lack of specialists is not the only problem persisting in regional hospitals. Senior level medical workers are mostly available in Yerevan. According to statistical data, there are 59 doctors per 10 000 people in Yerevan; the ratio in the regions is 3.5 times higher: only 17 doctors are available for the same number of population.
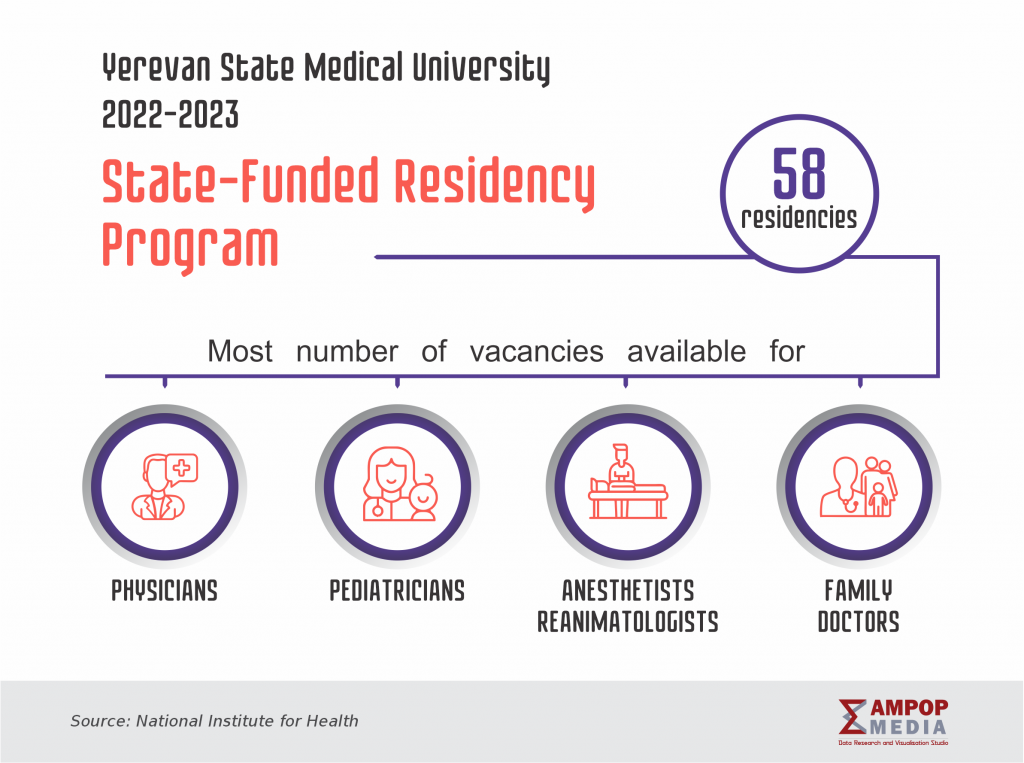
To fill the vacancies in regional medical centers, the Ministry of Health has started a clinical residency program at the Yerevan State Medical University since 2011; the program envisions tuition-free education in the departments of the university that train specialists in the disciplines most demanded in the regions.
Kristine Gyurjyan, the head of the Staff Management Department of the Ministry of Health, says the vacancies in the regions are announced twice a year in order to get a full picture regarding the most needed specializations. “We provide targeted clinical residency vacancies specifically for those disciplines, which are most wanted in the regions,” says Ms. Gyurjyan in a conversation with Ampop Media, adding that as part of the program the ministry signs a contract with the students, who apply for the mentioned places at the university.
The contract envisions an obligation on the part of the graduating student to work in a regional hospital for at least three-year period, as designated by the ministry.
Gyurjyan assures the program helps fill some 30 to 40 % of the vacancies in the regions.
Offering attractive terms of work in regional medical centers
The statistical data shared by the provost for postgraduate and continuous education of the Yerevan State Medical, Garnik Avetisyan, shows an interesting trend: this year alone, there have been 42 students majoring in pediatrics for their clinical residency program.
“The Ministry of Health has announced 22 vacancies for pediatricians on its official website as of the month of February, which could be filled shortly. The Muratsan University Hospital alone accepts some 1300 to 1400 children a week, which come from all over Armenia,” Avetisyan says. He adds, though, that the creation of work conditions more attractive than those offered in the capital is an urgency to meet the need of specialists in the regions.
Gyurjyan, too, tends to think that the reluctance of the young professionals to work in the regions has social underpinning. She believes, a young professional, especially the one with a family, looks for some satisfying living conditions and some interesting pastime options in order to agree to live away from the capital.
There were times when doctors were assigned to remote regions for a 5-year term; today, though, the numbers of vacancies have grown, whereas the contract period has dropped to 3 years.
“Our conversations with doctors prove 5 years are too long period for them, especially for those, who consider moving from Yerevan. People want some pastime [after work, which is hard to find] in the regions, and they face problems of organizing their routine. Those problems need to be solved when offering more attractive work and life conditions,” the representative of the Ministry of Health says.
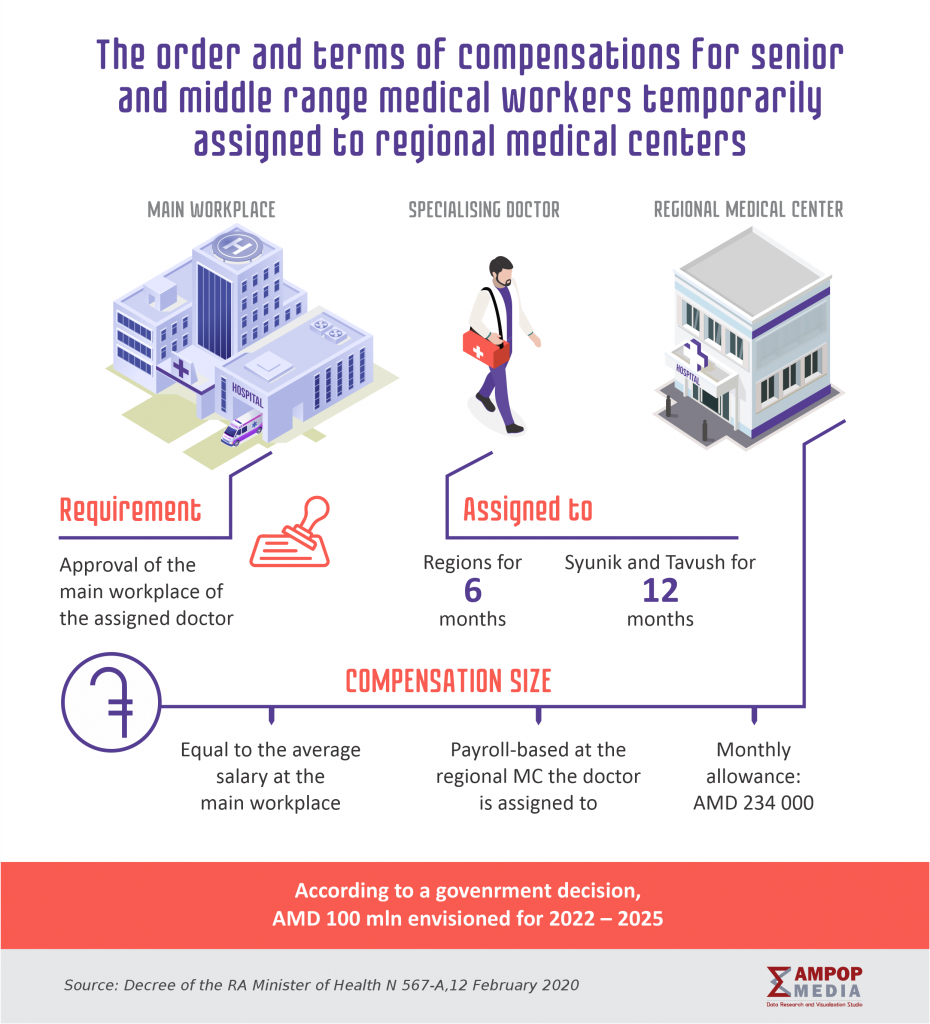
Another program, relaunched by the Ministry of Healthcare in 2020, which has the purpose of filling in vacancies in regional medical centers, offers more or less attractive terms of employment. The program is partially shown on the picture.
Eight specialists have been assigned to fill the open vacancies in medical centers in Kapan, Noyemberyan, Meghri, as well Tashir and Vanadzor.
The main specializations required at the regional medical centers include surgeons, anesthetists and emergency physicians, as well as obstetricians and gynecologists.
Kristine Gyurjyan says students oftentimes choose to major in disciplines that may prove potentially more profitable in future, or, alternatively, have wider scope of application. That is the reason that financially less attractive, yet highly demanded specializations are left out of the preference list.
Rebranding medical disciplines; might the COVID-19 have brought a positive change?
“Potential students were reluctant to choose emergency medicine. The salaries of emergency doctors have increased since the pandemic broke out, and students seem to opt for it more often. We have envisioned 12 targeted vacancies for clinical residency in emergency medicine, and have already managed to fill in even the pediatric emergency vacancies. The competition was high, because the specialization was made financially more appealing,” Gyurjyan says.
The provost of the Yerevan State Medical University believes the chosen majors shall meet the market expectations. To ensure employment opportunities, Avetisyan suggests limiting oversupplies in the job market.
“There are specializations that are both vital and interesting, but those are not perceived properly by the public, and, so, applicants opt for other specializations; those are forensic medicine or clinical pathology, for example. The applicants have quite vague understanding of the essence of the job and the opportunities it offers,” Avetisyan underlines.
Unlike pathology, which the management of the university has successfully promoted by revealing its attraction for applicants, forensic medicine still remains a less preferred discipline. There is no much demand for forensic medicine professionals in the market, despite a certain shortage of human resources.
The case is the same for epidemiologists and specialists in communicable diseases. The COVID-19 pandemic seems to have somewhat changed the public perceptions and the scope of applicants’ interests.
“Some specializations get more important in certain situations. There used to be few epidemiologists in recent years, yet, the COVID-19 showed that we live in time when epidemiologists are among the most highly needed globally. They are crucial in hospitals, too, for the prevention of epidemics, and also in terms of planning in times of emergencies,” Avetisyan stressed.
The pandemic has also proven the importance of pulmonologists.
Last year for the first time ever, the state funded clinical residency vacancies have been envisioned in angiosurgery, pulmonology, as well as thoracic surgery. In a conversation with Ampop Media, Gyurjyan observed that the war and the coronavirus pandemic showed the urge for these specializations.
To balance the supply and the demand in the market and to prompt the potential students to view options for majoring in disciplines beyond the trendy ones, the State Medical has undertaken some tactical steps by offering privileged terms for the professions on high demand. As part of these steps, the university has decreased the tuition for those who will choose pediatric specializations for about 50%.
In fact, the number of this year’s residencies points that the model of management chosen by the university does work. Finding ways of need-based distribution of graduates to clinics and medical institutions will be the next step of the efforts made in this direction.
by Lilit Poghosyan
Infographics by Anush Baghdasaryan and Karine Darbinyan
More articles about #AccesstoHealthCare
© All the stories, infographics and other visuals bearing the Ampop Media logo is possible to publish on other audiovisual platforms only in case of an agreement reached with Ampop Media and/or JFF.
Փորձագետի կարծիք
First Published: 10/11/2022